In a previous post, I introduced several models to study the cardiac human system. This first post introduced human aortic, brachiocephalic, carotid artery and coronary artery cells isolated by Cell Applications Inc. Here is the second part of this inventory of cellular models to study the human cardiac system, where I’ll be highlighting human internal thoracic artery, pulmonary artery, subclavian artery cells, cardiac fibroblasts and cardiomyocytes.
Later on, I’ll conclude this series by part III, referring to animal cellular models for studying the cardiac system. But let’s now concentrate on today’s topic!
Internal Thoracic Artery Cells
Human Internal Thoracic Artery Endothelial Cells

HITAEC have been used to investigate oral pathogens travel through the body by infecting dendritic cells and inducing them to migrate through endothelial layers by causing upregulation of CXCR4 (Miles, 2014). To identify genes that make Human Internal Thoracic Arteries resistant to atherosclerosis, HITAEC and HCAEC (derived from the athero-prone human coronary arteries, see previous post) were subjected to microarray analysis (Archaki, 2012). Twenty-nine genes were found to be expressed differently between HITAEC and HCAEC; one of them (TES) was shown to be downregulated in patients with coronary artery disease, resulting in increased monocyte adhesion, endothelial cell motility and transendothelial migration of monocytes.
Human Internal Thoracic Artery Smooth Muscle Cells
HITASMC are derived from the normal internal thoracic arteries (formerly called internal mammary arteries). HITASMC, along with Human Coronary Artery Smooth Muscle Cells, have been used to investigate the gene expression differences between smooth muscle cells from different arteries, underlying their differential response to injuries and proliferation stimuli (Lange, 2013).
Pulmonary Artery Cells
Human Pulmonary Artery Endothelial Cells

HPAEC provide an excellent model system to study many aspects of cardiovascular function and disease, including diabetes-associated complications, mechanisms of endothelial dysfunction caused by environment, oxidative stress, hypoxia and inflammation, as well as mode of action of various natural compounds and drug candidates.
HPAEC from Cell Applications, Inc. have been used to:
- Investigate vasculoprotective effects of propofol and show tat it induces Angiotensin-converting enzyme 2(ACE2) transcription via a PI3K-dependent mechanism, demonstrating its potential for treating pulmonary arterial hypertension (Cao, 2012);
- Analyze hits from a high-throughput screening assay and discover anziaic acid, from the lichen Hypotrachyna sp., as novel inhibitor for both Y. pestis and E. coli topoisomerase I (Cheng, 2013);
- Show that endothelin-1 that is released by endothelial cells during acute crisis in sickle cell anemia, increases vascular constriction (Ergul, 2004);
- Demonstrate that pollutant particles cause vascular dysfunction by up-regulating clotting-related genes, such as F2RL2, FOS, JUN, NF-kB, F2RL2, HMOX1 and tissue factor F3-mediated increase in IL-6 and IL-8 (Karoly, 2007), and activation of NADPH oxidase (Li, 2006) in endothelial cells;
- Demonstrate the central role of AMP-activated protein kinase (AMPK) in normal endothelial barrier function that is disrupted by exposure to lipopolysaccharides inhibiting AMPK, and causing endothelial hyperpermeability and lung injury (Xing, 2013);
- Confirm anti-inflammatory and cardioprotective effects of resveratrol by showing that it suppresses IL-13 and TNF-α induced eotaxin-1 gene expression, inhibits expression of JAK-1, reduces STAT6 phosphorylation and decreases p65 subunit of NF-κB (Yang, 2011);
- Determine that cGMP can prevent oxidant-induced damage to the endothelial barrier function by activating cGMP-dependent protein kinase PKGI through a Ca2+ independent mechanism (Moldobaeva, 2006);
- Demonstrate that exposure to radiation causes endothelial cells senescence (as judged by induction, downstream of mTOR, of senescence markers p53, p21/waf1, and senescence-associated b-Gal) due to up-regulation of proliferative signaling (IGF-1 and IGF-2 and hyperphosphorylation of IGF-1R) in the presence of cell cycle arrest (Panganiban, 2013);
- Show that vanadium exposure causes pulmonary vasoconstriction mediated in part by the inhibition of endothelial NO production via PKC-dependent phosphorylation of Thr495 of eNOS (Li, 2004);
- Evaluate, along with Human Dermal Microvascular Endothelial Cells (CADMEC) and Human Umbilical Cord Vascular Endothelial Cells (HUVEC), all obtained from Cell Applications, Inc., the cytotoxic effects of a novel pore-forming protein, proposed as an anti-tumor agent (Ellerby, 2013).
- Compare effects of BMP-4 on HPAEC and Human Coronary Artery Endothelial Cells (HCAEC, also from Cell Applications, Inc.) and showing that only in HCAEC BMP-4 treatment induced ROS, activated NF-kB, ICAM-1 and increased monocyte adhesiveness, explaining why its upregulation leads to atherosclerosis and hypertension in the systemic, but not pulmonary circulation (Csiszar, 2008);
- Demonstrate that macro- , but not micro-vascular pulmonary endothelial cells accumulate HIF-1 under hypoxic conditions (Fujiuchi, 2006);
- Confirm SPNS2 role as a transporter for S1P, a bioactive lipid, by monitoring S1P release from HPAEC and Human Umbilical Vein Endothelial Cells, both obtained from Cell Applications, Inc., and by showing that S1P was not released when SPNS2 was silenced with siRNA (Hisano, 2013). Additionally, quantitative real-time PCR indicated that Spns2 mRNA was transcribed at higher levels in venous HUVEC compared to arterial HPAEC, suggesting heterogeneity in the expression level of SPNS2 among different vascular beds.
Note that several publications describe the differences between endothelial cells from different vascular beds (Csiszar, 2008, Hisano, 2013) and between micro- and micro-vascular cells from the same organ (Fujiuchi, 2006), highlighting the importance of confirming any new findings on cell lots obtained from several different origins. tebu-bio offers the widest variety of endothelial cells, and is well equipped to meet this need.
Human Pulmonary Artery Smooth Muscle Cells

HPASMC from Cell Applications, Inc. have been used to show that IL-22 promotes the growth of pulmonary vascular SMCs via a signaling mechanism that involves NADPH oxidase-dependent oxidation (Bansal, 2013). Inducers of pulmonary hypertension, characterized by thickened pulmonary arterial walls, activate expression of anti-apoptotic Bcl-xL gene via binding of GATA-4 to its promoter; the activation can be suppressed by targeting gata4 gene transcription (Suzuki, 2007). Serotonin induces growth of Pulmonary Artery Smooth Muscle Cells and is able to transactivate the BMP receptor in pulmonary artery SMCs, leading to activation of Smads 1/5/8 via Rho and Rho kinase pathway (Liu, 2009). Pulmonary Artery Smooth Muscle Cells growth can be suppressed by trans-retinoic acid by inducing expression of GADD45A, a known cell growth suppressor, downstream of the retinoid acid receptors RARalpha, RARbeta, RARgamma, RXRalpha, and RXRbeta, indicating possible involvement of retinoic acid in pulmonary vascular remodeling (Preston, 2005). Treatment of Pulmonary Artery Smooth Muscle Cells with plasma containing reduced levels of all-trans RA and 13-cis RA promoted cell growth (Day, 2009). Retinoic acid was also shown to inhibit migration of pulmonary smooth muscle cells by inhibiting PI3K/Akt-dependent reorganization of actin cytoskeleton (Day, 2006). Pulmonary Artery Smooth Muscle Cells from Cell Applications, Inc. were also used to study effects of iron chelation on vascular remodeling and its implications for development of pulmonary hypertension as a result of ROS activity (Wong, 2012). Finally, this cells were used to show that antitumor drugs can selectively target remodeled pulmonary vessels, but not normal vessels (Ibragim, 2014).
Subclavian Artery Cells
Human Subclavian Artery Endothelial Cells

HScAEC, along with human aortic (HAOEC), carotid artery (HCtAEC), coronary artery (HCAEC) and brachiocephalic artery (HBcAEC), all from Cell Applications, Inc., have been used to demonstrate that not only blood vessels from different tissues are highly heterogeneous, they also interact differently with leukocytes during the inflammation response (Scott, 2013). The authors further showed that differential N-glycosylation of commonly expressed vascular adhesion molecules may be responsible for this heterogeneity, as well as for modulation of signaling under resting and activated inflammatory conditions. This also explains why specific vascular beds may be more or less susceptible to particular diseases or stimuli. Importantly, if cells from different sources were used, these results could not be convincingly validated due to a number of uncontrolled variables, such as age, race, genetic variability or life style choices of the donors. To eliminate the donor-to-donor variability, the scientists took advantage of the great variety of primary cells offered by Cell Applications, including the option of ordering a panel of endothelial cells obtained from different vascular beds of the same donor!
Human Subclavian Artery Smooth Muscle Cells
HScASMC provide a useful in vitro system to study all aspects of cardiovascular function and disease, especially those related to mechanisms of hyperplasia and hypertrophy of intimal smooth muscle cells leading to vascular occlusion.
Cardiac Fibroblasts
Human Cardiac Fibroblasts
Cardiac fibroblasts are the most prevalent cell type in the heart, making up 60-70 % of all cells. HCF provide an excellent model system to study many aspects of human heart function and pathophysiology.
HCF from Cell Applications, Inc. have been utilized in a number of research publications, for example to:
- determine that electrical coupling between cardiomyocytes and fibroblasts is mediated by large-conductance Ca2+-activated K+ channels that can be stimulated by estrogen receptor agonists (Wang, 2006, 2007); and show that antimitogenic effects of estradiol on HCF growth are mediated by cytochromes 1A1/1B1-and catechol-O-methyltransferase-derived metabolites (Dubey, 2005);
- show that in response to mechanical stretch, cardiac fibroblasts release TGF-β which causes trombomodulin downregulation, increasing the risk of thromboembolic events (Kapur, 2007) and also induces cardiac fibroblast differentiation into myofibroblasts via increased Smad2 and ERK1/2 phosphorylation, that could be stimulated by endothelin-1 and inhibited by Ac-SDKP (Peng, 2010);
- demonstrate that activation of G protein-coupled receptor kinase-2 (GRK2) prevents normal regulation of collagen synthesis in cardiac fibroblasts mimicking heart failure phenotype (D’Souza, 2011); identify FGF2 signaling pathway as potential target for modulating apoptosis in cardiac pathology (Ma, 2011) and investigate the roles of scleraxis (Bagchi, 2012) and AMPKα1 (Noppe, 2014) in scar formation following myocardial infarction;
- show that the KATP channel opener KMUP-3 preserved cardiac function after myocardial infarction by enhancing the expression of NO synthase and restoring MMP-9/TIMP-1 balance (Liu, 2011).
HCF from Cell Applications, Inc. were also shown to express delayed rectifier IK, Ito, Ca2+-activated K+ current (BKCa), inward-rectifier (Kir-type), and swelling-induced Cl- current (ICl.vol) channels (Yue, 2013).
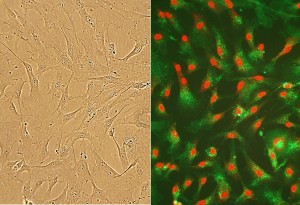
Cardiomyocytes, iPS derived
ReproCardio 2 Human iPSC-derived cardiomyocytes have been extensively characterized for their functional responsiveness to the known cardiotoxic compounds. In all our tests, including assays of cardiotoxic compounds not correctly identified by the hERG assay, ReproCardio has generated results in complete agreement with clinical findings.
In a previous post, I highlighted the characterisation of ReproCardio 2 cardiomyocytes and illustrated the applications they are used for.
Primary cells for research
Because of the complex heterogeneity that exists not only between different donors, but even between different vascular beds in the same individual, it would be prudent to confirm any new findings on primary cell lots coming from several different origins.
To illustrate this, Scott et al. (Scott, D.W., M.O. Vallejo, and R.P. Patel. 2013. Heterogenic endothelial responses to inflammation: role for differential N-glycosylation and vascular bed of origin. Journal of the American Heart Association. 2:e000263-e000263) demonstrated that not only blood vessels from different tissues are highly heterogeneous, they also interact differently with leukocytes during the inflammation response using HCAEC, HAOEC, HCtAEC, HScAEC and HBcAEC (Cell Applications Inc.). The authors further showed that differential N-glycosylation of commonly expressed vascular adhesion molecules may be responsible for this heterogeneity, as well as for modulation of signaling under resting and activated inflammatory conditions. This also explains why specific vascular beds may be more or less susceptible to particular diseases or stimuli. Importantly, if cells from different sources were used, these results could not be convincingly validated due to a number of uncontrolled variables, such as age, race, genetic variability or life style choices of the donors. To eliminate the donor-to-donor variability, the scientists took advantage of the great variety of primary cells offered by Cell Applications, including the option of ordering a panel of endothelial cells obtained from different vascular beds of the same donor!
It’s important to find a reliable source, and preferably one offering a large selection of cell types and associated media, for whatever technical application and thematics you’re working on: flow based assays, primary and secondary screening, stem cell studies, diabetis & obesity, cosmetology, electrophysiology, cell imaging, bio-banking…
Points to bear in mind… you want to be sure of getting:
- Access to large and regularly updated lot inventories
- Same cell types from various species
- Arrays of cell types from the same donors
- Lot reservation pending testing & validation
Which cell types are you looking for? The tebu-bio group (their headquarters are in France, but one of their local specialists across Europe is bound to be near you!), offer among their broad range of products: Islet cells, sebocytes, neurones, endothelial & epithelial cells, cardiomyocytes, fibroblasts, keratinocytes, melanocytes…
Get in touch with their Cell Specialists to learn more!